Chiropractic care is regarded as one of the safest, drug-free, non-invasive health care delivery methods when it comes to treating a variety of neuromusculoskeletal conditions including headaches, neck pain, back pain and joint pain in the arms or legs. Chiropractic adjustments are used to restore alignment, optimize range of motion, reduce muscle spasm and tension, and promote optimal balance and tone of the nervous system. As with any healthcare delivery system, there is always a possibility for adverse side-effects, although chiropractic care has earned an excellent safety record as evidenced in recent scientific evidence and literature.
Many patients feel immediate relief following chiropractic adjustments, although some patients may experience mild soreness or stiffness, a headache or fatigue following an adjustment. These symptoms are comparable to what someone may experience after starting a new exercise program and typically resolve within 24 hours.1
Not only is chiropractic care safe, it is equivalent or superior to traditional medical care including physical modalities, medication, education or exercise in regards to getting people with acute low back pain back on their game according to a study published in Spine in 2010. These benefits were observed at both short-term and long-term follow up. A study in the Annals of Internal Medicine found that spinal manipulative therapy and exercise are more effective at relieving neck pain than pain medication.2
Neck Adjustments
Chiropractic neck adjustments can include a high-velocity, low-amplitude spinal manipulation to the cervical spine which can be very effective in treating neck pain and certain types of headaches. While this is a very safe procedure, some reports have associated cervical spinal manipulation with certain types of stroke following a cervical artery dissection (tear). The largest study3 examining the association of cervical spine manipulation and stroke came out in 2008 demonstrating that patients are no more likely to suffer from a stroke following a cervical spinal manipulation as they are by visiting their primary care physician. In fact, there are many studies examining millions of patients demonstrating no greater association of stroke for persons under chiropractic care compared with people under medical care. The study also concluded that this arterial tear is a very rare event and can occur spontaneously in seemingly healthy, middle-aged persons during everyday activities such as swimming, or turning your head while driving, or while having a hair shampoo at a salon. This study concluded there is no causal relationship between neck manipulation and stroke.
Association Vs. Causation
It is important to understand the difference between association and causation. People experiencing a cervical artery dissection may experience neck pain or a headache leading them to seek help from a healthcare professional- typically a chiropractor or primary care physician, but the help they seek is not the cause of the artery dissection. The current research and literature reports the occurrence of cervical artery dissection associated with visiting your chiropractor or primary care physician is 1 case for every 5.85 million visits.
In February 2016, a team of neurosurgeons at the University of Pennsylvania Hershey Medical Center published research4 concluding, “There is no convincing evidence to support a causal link between chiropractic manipulation and cervical artery dissection (CAD).”
Comparatively Speaking
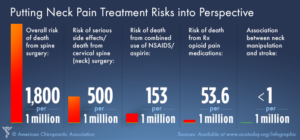
It is also important to compare the risks of other common modalities used to treat neck pain and headaches. Prescription and over-the-counter non-steroidal anti-inflammatories (NSAIDs) such as ibuprofen and aspirin are responsible for one third of all hospitalizations and deaths related to gastrointestinal bleeding according to a study from the American Journal of Gastroenterology.5 There are over 16,500 NSAID related deaths in the United States every year.
As many as one in four people who receive prescription opioids long term for non-cancer pain in primary care settings struggle with addiction.6 Moreover, the CDC has classified the abuse of prescription opioid pain medications in the U.S. as “epidemic.” In 2014, more than 28,500 people died as a result of taking these drugs.
Putting all of this into perspective, here are the risk factor ratios for the most common treatments available to treat neck pain:
Amongst all health care providers, chiropractors have some of the lowest malpractice insurance premiums across the board. This is another indicator of the relative safety of chiropractic care.
Red Flags To Share With Your Doctor
It is important to share with your doctor any new or different details about neck pain and headaches you have been experiencing, especially if it is a different type of pain or if the intensity is significantly more intense than previous episodes or if you have had any injuries. Also, any associated symptoms such as dizziness, nausea/vomiting, visual changes, difficulty with swallowing or speech or loss of balance should be reported to your health care professional immediately or seek evaluation at your nearest emergency room as these associated symptoms may be red flag warnings to the onset of a more serious problem.
1. Senstad O, et al. Frequency and characteristics of side effects of spinal manipulative therapy. Spine 1997 Feb 15;435-440.
3. Cassidy D, et al. Risk of Vertebrobasilar Stroke and Chiropractic Care. Spine 2008; 33:S176–S183.

Recent Comments